Eligible NHS patients missing out on new medicines that could extend lives and add £billions to the UK economy
- Analysis of just four disease areas shows approximately 1.2 million eligible patients are currently missing out on NHS treatments
New research by PwC for the ABPI published today sets out the potential benefits of increased investment in clinically- and cost-effective new medicines to patients, society, and the economy.
Investment in medicines is already creating more efficient and effective health services in countries around the world, resulting in better health outcomes and improved survival rates. We should be striving for the same. Richard Torbett, Chief Executive, ABPI
The research reveals how improved use of 13 medicines across four treatment areas – stroke prevention, kidney disease, asthma, and type 2 diabetes - can transform patient care and add billions of pounds to the UK economy through increased productivity over patients’ lifetimes.
It shows:
- An estimated 1.2 million additional NHS patients are currently eligible for - but are missing out on - these medicines. This population is greater than the combined populations of Glasgow, Swansea, and Sunderland.
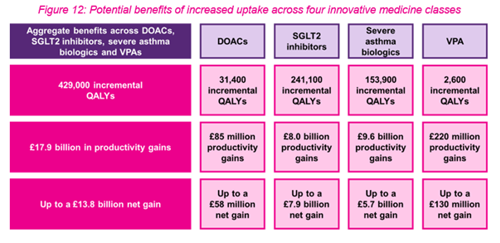
- In aggregate, extending the use of these medicines would provide patients with more than 429,000 additional years living in good health (QALYs).
- £17.9 billion in productivity gains would accrue to the UK economy.
- £5.5 billion of which could be paid directly back to the exchequer through taxes from increased paid labour productivity.
These productivity gains would more than offset the incremental costs of increased uptake.
The move could also help to tackle health inequalities and help deliver on the government’s Levelling Up agenda. Many major causes of morbidity and mortality, including asthma, disproportionately impact people from lower socioeconomic backgrounds, for example.
Increasing the use of certain medicines for type 2 diabetes stands to bring the biggest gain to patients, adding an estimated 241,100 extra good quality years to patients’ lives, as well as an estimated £8 billion to the economy in productivity, over patients’ lifetimes.
Increasing the use of medicines for severe asthma patients stands to bring the biggest gain to the economy, with an estimated £9.6 billion to be gained by the UK economy in productivity, while adding an estimated 153,900 extra good quality years to patients’ lives.
DOACs – Direct Oral Anticoagulants – can prevent hospitalisations for deep vein thrombosis and pulmonary embolism as well as reduce the acute and long-term care required for stroke patients, freeing up staff and the need for outpatient anticoagulant clinics across the UK.
Increasing their use alone would provide an estimated 31,400 years of better quality for patients and deliver an estimated £85 million in productivity gains to the economy.
The report highlights three key challenges to address to improve patient outcomes and to ensure the UK’s status as a priority launch market for new medicines remains:
- Breadth of access: UK patients have lower access to innovative medicines than patients in other comparable countries. Between 2015-2019, of the positive recommendations made by NICE (i.e., decisions that a new medicine should be available on the NHS), 43 per cent have been limited to narrower populations than recommended by the UK and European regulators. Of these, 65 per cent were approved for half the number recommended and 35 per cent were given to less than a quarter of patients in the UK than elsewhere.[1]
- Speed of access: From licensing to first use of a new medicine by NHS England the average wait time is almost 11 months (335 days). In contrast patients in Germany can typically expect to receive a new medicine almost three times faster (120 days). England falls 7th among comparator countries with Scotland 11th.[2]
- Extent and rate of uptake: The government’s own analysis shows that for over 75 medicines recommended by NICE and launched between 2013 and 2019, the UK per-capita use in the first five years post launch was 64 per cent of the average of 15 comparator countries.[3]
The case for investing in innovative medicines is clear, yet from the macroeconomic perspective, the UK spends the lowest by GDP of any of the G7 nations. In stark contrast, the UK spends less per capita on pharmaceuticals than 9 of its peer high-income countries: the United States, Germany, Japan, France, Australia, Spain, South Korea, Italy, and Canada.
This means that for every £100 in GDP, the UK spends just 81p on pharmaceuticals, compared to £2.35 in the US, £1.94 in Germany and £1.84 in Japan.
The report underlines how the severe impact of the pandemic and low investment in the latest medicines and therapies has compounded existing challenges; with existing research showing that patients in the UK face lower survival rates for conditions including cancer, COPD, and stroke than patients in similar developed countries.
Analysis from 2020 shows that for breast cancer survival rates, the UK ranks 14th out of 18 developed countries and 15th for cervical cancer. For colon cancer, the UK is bottom.
Analysis from 2016 shows that the UK patients had 50 per cent higher YLL (years of life lost) due to ischemic heart disease than France or Spain and more than double the YLL rates for chronic obstructive pulmonary disease (COPD) than Finland or France.[4]
The UK had 60 per cent higher YLL rates for lung cancer compared to Finland or Sweden, both who have substantially higher uptake than the UK in the leading medicines for lung cancer treatment.[5]
With the next wave of innovative medicines in the pipeline – more than 30,000 new clinical trials have started since 2015 – more ground-breaking advances can bring a step-change in health outcomes in the coming years. The report suggests that pharmaceutical innovation will continue to be an important driver of the health and wealth of the UK.
Richard Torbett, Chief Executive of the Association of the British Pharmaceutical Industry, said:
“The pandemic has starkly highlighted the relationship between the health of the population and the health of the economy. Medicines and vaccines are playing a vital role in getting us all back to work.
This report shows how we can use the experience from COVID to prevent and treat other diseases which create a drag on the economy. The evidence is clear; providing patients with the medicines they are eligible for will help people live longer, healthier lives, while growing the economy and increasing tax receipts for the government.
Investment in medicines is already creating more efficient and effective health services in countries around the world, resulting in better health outcomes and improved survival rates. We should be striving for the same.”
#ENDS#
[1] OHE, 2020
[2] EFPIA W.A.I.T. Indicators, 2021
[3] OLS, 2021
[4] Public Health England, 2020
[5] IHE, 2020
- Health and Access to Medicines
Last modified: 20 September 2023
Last reviewed: 20 September 2023
-
PwC - Transforming lives raising productivity
Download